Prescription Drug Costs: Trends and Insights into Private Drug Plans
Given that the cost of prescription drug coverage is currently a topic of national conversation, the yearly publication of Express Script Canada’s Drug Trend Report couldn’t have arrived at a better time.
If you’re looking for insights into the drivers of cost as well as solutions to help manage benefit plan affordability, the report contains a wealth of instructive data.
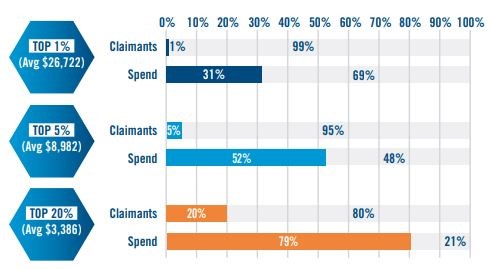
One of the top-order findings is that a small number of benefit claimants are responsible for a majority of costs: approximately 20% of claimants represent 80% of total spending costs.
Another key finding involves the proportion of drug costs arising from speciality medications: whereas in 2008 speciality drugs accounted for only 15% of the total drug spend, they now account for 31% of all drug spending. This is especially noteworthy when considering that innovations in the drug development pipeline suggest the possibility of further increases in the use of high-cost specialty medications, moving forward.
Containing the escalating costs of specialty medications is a significant challenge for benefit providers: increased costs can lead to concerns regarding balancing patient access and benefit affordability.
More broadly, drug costs have been on a steady upward trajectory, with a 2.5% year-over-year increase from 2015-2016.
Read: The Value of Health Insurance
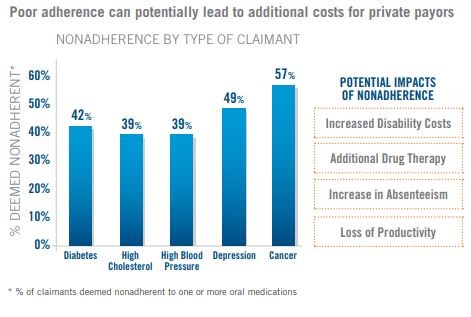
There are also concerning trends with respect to adherence in terms of costs and health outcomes: it’s well-understood that nonadherence to medication regimens can lead to negative consequences: greater risk of additional health problems, increased absenteeism from work, and a higher risk of disability. It’s a problem across many different disease states and can be a real barrier to achieving good health.
A significant conclusion within the Drug Trend Report is the fact that comprehensively managed pharmacy benefit plans can help contain costs while also optimizing therapies. Holistic treatment protocols aim to provide support and guidance to patients so that they are only taking appropriate medications and taking them as prescribed.
Benefit plan providers make use of a variety of clinical tools to ensure that the right patient is receiving the right therapy at the right time. These tools are critical components of comprehensively managed benefit plans:
- Intelligently designed formulary to optimize drug therapies
- Behavioural science to inform how patients are engaged in their health
- Patient health management services to offer expert advice on drug use
Looking ahead down the drug development pipeline, the report notes that there is great therapeutic promise for gene-based therapy, yet such emerging therapies will come at great cost. Given that high-cost therapies promise to be one of the main drivers of benefit spending in the years to come, benefit plan providers and plan sponsors will continue to seek targeted support solutions that contain costs and promote healthier outcomes.
You can read the full report here and see how comprehensively managed benefit plans can help balance cost and care effectively.