A strategic approach to safeguarding prescription drug benefits
In the face of a rapidly changing pharmacy landscape, many plan sponsors are struggling to maintain the valued drug benefit they offer their employees.
The challenges are formidable, with increasing costs for traditional drugs and mounting financial risks associated with specialty drug claims. Spending on high-cost prescription drugs continued to grow at alarming rates in 2015, with new treatments introduced at staggering prices (such as a drug for genotype 1 of the hepatitis C virus, range from the lower end – $47,000 if drug is prescribed for eight weeks – to as high as $268,000 if combination therapy is required for 24 weeks). A long list of high-cost medications currently in development further intensifies the financial risk plan sponsors face.
Read: Exorbitantly priced drugs challenge Canadian families, benefit plans
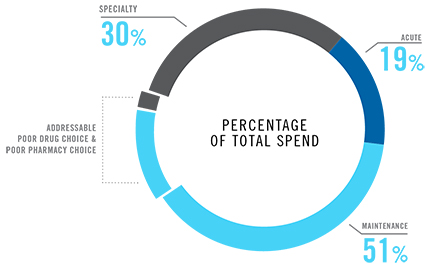
But there are proven ways to protect the prescription drug benefit. For example, our research shows that up to $1 in every $3 spent on maintenance medications does not improve patient health outcomes. Active benefit management helps members make more effective decisions, driving this waste – billions of dollars each year – out of the system.
Our 2015 Drug Trend Report also found that patient adherence – always a major concern among health-care professionals – declined as patients received medications from multiple pharmacies. These findings illustrate the challenges that patients face when managing multiple medications.
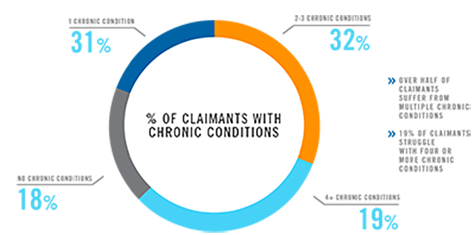
These challenges are even greater for patients with multiple or complex conditions, a group of just 19% of claimants accounted for 53% of total spending in 2015. Their average annual per patient spending was $2,296 in 2015, 4.7 times that of other claimants.
Active benefit management and pharmacy solutions that provide counselling and services, side effect management, specialized expertise and coordination of care have proven invaluable in helping these patients manage their health.
Mapping a strategic approach
At Express Scripts Canada, we leverage insights gained by managing claims for more than seven million Canadians to design solutions that make the use of prescription medications safer and more affordable.
These innovative solutions integrate actionable data, behavioural science techniques, clinical expertise and patient support tools, and are proven to help plan members manage their health and make better decisions.
For example:
- The Express Scripts Canada Dynamic Therapeutic Formulary helps to educate members about the cost of drugs and empowers them to be involved in choosing those drugs that are both clinically effective and cost effective.
- Express Scripts Canada’s Prior Authorization program confirms that high cost drugs are prescribed for the treatment of Health Canada-approved indications and are used according to standards of care. This helps control costs overall and allows the plan to continue to cover high cost drugs for plan members who need them by ensuring the right drug is dispensed to the right person at the right time.
- At the very centre of the Express Scripts Canada strategy are pharmacists who serve as proactive member advocates. Express Scripts Canada Pharmacy helps members understand and make better decisions about their maintenance medication options. Free delivery, auto refills and reminders and other tools make it easier for them to take medications as prescribed.
Our ongoing data analysis proves that these innovative solutions drive better patient decisions, lower costs and result in healthier outcomes – protecting the sustainability of the prescription drug benefit in the process.